Case #15: Too Much Digoxin
Author: Neeraj Chhabra, MD
Peer Reviewer: Christopher Hoyte, MD
An 86-year-old female was brought in by her family for recurrent episodes of syncope over the past 7 days. She has a past medical history of hypertension and heart failure and takes metoprolol, enalapril, furosemide, and digoxin. Her primary physician recently increased her furosemide dose to 80 mg PO BID. Her exam is remarkable only for mild abdominal tenderness.
Vitals: Temp: 98.4, HR: 60, RR: 18, BP: 134/87, O2 Sat: 99% on RA
Labs were sent from triage and revealed a digoxin level of 2.2, a creatinine of 3.0 (baseline 1.3), and a K of 3.2. The remainder of her labs were within normal limits.
What are the common symptoms suggestive of digitalis toxicity?
CNS: Confusion, Altered mental status, or Syncope
HEENT: Yellow/Green Visual “halos”
Cardiovascular: Palpitations, PVCs, Bradyarrhythmias, or Tachyarrhythmias
GI: Dyspepsia, Abdominal discomfort, Nausea, Vomiting
What are some classic ECG findings associated with digitalis toxicity?
-Scooping of the ST segment (Note: this can be seen even with therapeutic levels)
-Junctional tachycardia
-Atrial Fibrillation with slow ventricular response
-Bidirectional ventricular tachycardia (pathognomonic for digoxin toxicity)
-Paroxysmal atrial tachycardia with variable blocks (pathognomonic for digoxin toxicity)
What is the mechanism of action of digitalis and its toxicity?
Digitalis inhibits the membrane protein Na-K ATP-ase pump. Its use results in increased intracellular sodium, decreased extracellular potassium, and increased calcium availability to cardiac myocytes. In toxicity, arrhythmias originate from increased excitability due to lowered resting potential and slowing of conduction through the AV node.
What factors commonly induce toxicity in patients taking chronic digoxin?
-Acute or worsening renal failure
-Hypokalemia
-Hypomagnesemia
-Hypercalcemia
-Concomitant use of amiodarone, verapamil, quinidine, macrolides, or cyclosporine due to inhibited renal clearance.
Besides Digoxin, what are some other digitalis containing substances?
-Oleander
-Foxglove
-Lilly of the Valley
-Red Squill
-Rhododendron
-Bufo sp. toad venom (contains hallucinogens and digitalis)
What are the treatment options for bradydysrhythmias?
-Atropine (0.5-2.0 mg IV)
-Transcutaneous or transvenous cardiac pacing
-Anti-digoxin Fab fragments (Digibind™)
What are the treatment options for ventricular dysrhythmias?
-Magnesium sulfate (2-4 g IV)
-Fosphenytoin (15mg PE/kg) – depresses ventricular automaticity
-Lidocaine (1mg/kg)
-Anti-digoxin Fab fragments (Digibind™)
What are the indications for using Digibind™?
-Ventricular dysrhythmias
-Severe hypotension
-Hyperkalemia greater than 5.5 mEq/L
-Bradydysrhythmias that are unresponsive to atropine
Note: Digoxin is not effectively dialyzable due to its large volume of distribution.
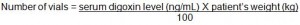
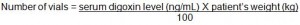
How is the dose of Digibind™ calculated?
Digibind™ is stored in vials. To calculate to number of vials needed for toxicity use the formula below:
What are two common errors when measuring Digoxin levels?
1. Measuring a Digoxin level too early post-ingestion.
-Digoxin levels are often falsely elevated when checked within 1-2 hours post-ingestion due to incomplete distribution. Ideally, levels should be checked six hours post-ingestion
2. Checking a Digoxin level after giving Digibind.
-Do not check a Digoxin level after giving Digibind. The Digoxin level detects both bound and unbound Digoxin, so it will be falsely elevated due to the bound Digoxin and does not guide clinical management.
References:
Kelly RA, Smith TW. Recognition and management of digitalis toxicity. Am J Cardiol. 1992 Jun 4;69(18):108G-118G
Ma G, Brady WJ, Pollack M, et al. Electrocardiographic manifestations: digitalis toxicity. J Emerg Med. 2001 Feb;20(2):145-52.
Pita-Fernández S, Lombardía-Cortiña M, Orozco-Veltran D, et al. Clinical manifestations of elderly patients with digitalis intoxication in the emergency department. Arch Gerontol Geriatr. 2011 Sep-Oct;53(2):e106-10.
Yang EH, Shah S, Criley JM. Digitalis toxicity: a fading but crucial complication to recognize. Am J Med. 2012 Apr;125(4):337-43.
Return to Case List